Hospitals around the world are recognising the benefits of switching to single-use, but why?
Simply put, switching to single-use devices and surgical instruments reduces the risk of patient-to-patient cross- contamination as well as saving the time and cost involved in reprocessing.
Reusable instruments can offer false economies to healthcare practitioners and pose an inherent concern in relation to their maintenance, storage and repeated use.
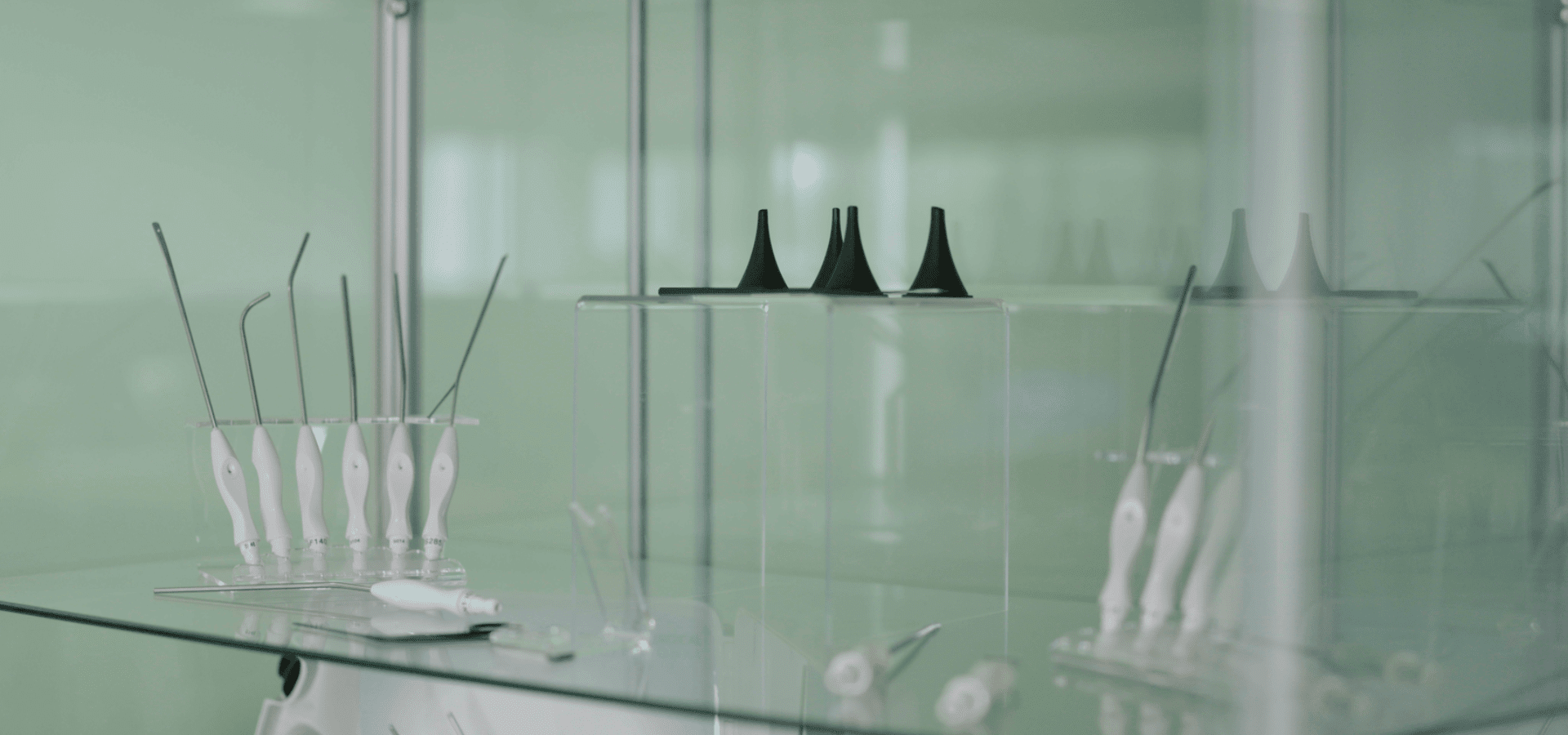
By adopting single-use instruments, healthcare practitioners can effectively eliminate all the above issues with a single decision. These are designed to be cost-effective, completely sterile and ready to use at the point of care.
Reusable Instrument Problems
What are the common issues that can arise when using reusable devices?
Washing and Rinsing
Failed Inspections
Missing Instructions
Assembly Problems
Untrained Staff
Unsterile Storage

Cost Reduction
One of the most significant hidden costs associated with reusable surgical instruments is that they can contribute to cross-contamination between patients.
Financial Strain
Cross-contamination causes more financial strain on healthcare practitioners and institutions when
having to treat such infections after the post-operative stay.
Surgical Site Infection
Another unconsidered cost is the reduction in capacity to treat other patients, creating a further
inefficiency within healthcare systems.
Hidden Costs
Reusable instruments can have hidden costs that are not reflected in the purchase price.
The unit price for reusables at the point of purchase does not reflect these additional costs. These include reprocessing costs, transportation costs, instrument repairs and the cost of lost instruments – all of which can have a significant impact on hospital budgets.
Single-use surgical instruments do not entail any of these additional costs. The cost of use is clear and defined at the cost of purchase, ultimately saving money.
Time Savings
Reprocessing time is frequently underestimated, especially when extra time must be allocated when trying to clean fine cannulated instruments.
Factors which consume valuable sterile services and clinical time include workflow disruption, tracking and tracing lost instruments, postponed surgeries caused by dirty or missing instruments, in addition to the repair of devices.
Logistics
The storage, monitoring, cleaning and transportation of reusable surgical instruments all incur
activity and time. Single-use instruments only need to be transported, then safely disposed of
to ensure optimal theatre workflow efficiency. If surgical instruments are designed for repeated use,
the logistics involved in their management incur an increased risk of them being mislaid or
kept at different sites.
Instrument Tracking
Healthcare institutions often adopt very costly and time-intensive tracking systems to ensure that reusable instruments can be easily located and identified.
Personnel
Reusable instruments require personnel to clean, repair, store and transport them. This activity could be spent on other duties in a healthcare institution, which would increase efficiency across the board.
Single use instruments are guaranteed sterile when packaged, saving time to the institution. They are ideal as a backup to reusable instruments in the OR, and provide an easy, quick alternative in case of delays or biohazard.
Risk Reduction
We recognise there is a time and place for reusable surgical instruments, but healthcare practitioners incur an unnecessary risk to their patients by using instruments that are difficult to clean with standard sterilisation methods.
The greatest risk is that of cross-patient contamination due to reusable surgical instruments not being adequately cleaned or maintained.
A Growing Concern
Device Reprocessing
This has been repeatedly linked to residual contamination left by reprocessing agents that fail to enter difficult-to-reach areas of reusable devices. The breakdown of device materials can result in often imperceptible damaged areas which act as breeding grounds for infection. Over time, wear and tear on reusable surgical devices can compromise functionality of the device.
Health Risks
Reprocessing procedures can expose healthcare workers to toxic chemicals. Such substances can also pose risks to the patient themselves in surgery, if the cleaning process was not thorough, or incorrectly followed on the surgical instrument.
The risks associated with the reprocessing of instruments is eliminated when using disposable instruments, as devices have not been used on other patients, or in prior procedures.
Have any questions about the benefits of disposable instruments?
Contact us below, and we will try our best to field your enquiry.